Scroll to:
Features of component body composition in children with infantile cerebral palsy
https://doi.org/10.37489/2949-1924-0104
EDN: ZIWMJL
Abstract
Relevance. Nutritional status disorders are common in patients with cerebral palsy (CP) and are caused by multiple factors related to the disease and its complications. They aggravate the underlying disease, reduce the quality of life, and decrease rehabilitation effectiveness.
Objective. To study the body composition characteristics of children with CP using bioimpedance analysis.
Materials and methods. Body composition parameters were studied to assess the nutritional status of 100 children with CP.
Results. The study revealed significant differences in body composition in children with CP associated with nutritional deficiencies. Latent changes in body composition were detected in children without physical developmental delays. Follow-up after 12 months confirmed a progressive decrease in the active cell mass, lean body mass, and skeletal muscle mass in patients with CP.
Conclusions. Children with cerebral palsy have been shown to have significant changes in body composition, including decreased muscle and fat mass, which progress over time even with normal anthropometric parameters.
Keywords
For citations:
Leontiev I.A., Sitnikova E.P., Uspenskaya T.L., Olendar N.V., Kovina M.V. Features of component body composition in children with infantile cerebral palsy. Patient-Oriented Medicine and Pharmacy. 2025;3(3):63-68. (In Russ.) https://doi.org/10.37489/2949-1924-0104. EDN: ZIWMJL
Relevance
Cerebral Palsy (CP) is a socially significant disease, ranking second in the structure of childhood disability [1]. It is also a serious pediatric problem due to its high prevalence, early onset of disability, and significant deterioration in patients' quality of life [2]. In addition to motor impairments characteristic of the core disease, these children often suffer from musculoskeletal, digestive, and endocrine system issues, which collectively contribute to the development of nutritional deficiencies. The presence of these deficiencies, in turn, reduces the effectiveness of rehabilitation, which typically focuses precisely on motor skills.
The prevalence of nutritional disorders in this patient group varies widely and, according to literature, can reach up to 70% [3, 4, 5]. The high frequency of nutritional disorders is largely due to the severity of the neurological deficit, significant motor limitations [6], and the presence of dysphagia [7].
In children with CP, nutritional insufficiency develops under the influence of multiple factors, including difficulty eating, impaired chewing and swallowing, gastrointestinal manifestations (such as gastroesophageal reflux and constipation), and metabolic disturbances associated with altered metabolism. All this leads to deficiencies in macro- and micronutrients, reduced muscle mass, and delayed physical development, which, in turn, exacerbates the underlying disease and worsens the patients' quality of life. Timely diagnosis and correction of the nutritional status in children with CP play a key role in improving their overall condition, enhancing the effectiveness of ongoing rehabilitation, and helping to prevent complications [8].
Objective
To study the characteristics of the body composition in children with CP using bioimpedance analysis.
Materials and Methods
The study of body composition was conducted in children diagnosed with CP receiving treatment at the Yaroslavl Regional Children's Clinical Hospital. The mean age of the children was 8.7 ± 3.3 years (n=100), of whom 38% (n=38) were male and 62% (n=62) were female. A brief characteristic of the group is presented in Table 1.
Assessment of anthropometric indicators was performed using specialized standards for children with CP (Life Expectancy Project, 2011) [9]. The severity of CP was determined using the GMFCS (Gross Motor Function Classification System) [10].
Table 1. Characteristics of the Studied Group of Children with Cerebral Palsy (n=100)
| CP Form (abs. /%) | Distribution by Motor Level (GMFCS) (abs. /%) | Clinical Severity Assessment (abs. /%) | |||
|---|---|---|---|---|---|
| Spastic Diplegia | 58/58% | GMFCS 1 | 24/24% | Moderate | 60/60% |
| Hyperkinetic | 12/12% | GMFCS 2 | 26/26% | ||
| Hemiparetic | 18/18% | GMFCS 3 | 32/32% | Severe | 40/40% |
| Double Hemiplegia | 8/8% | GMFCS 4 | 6/6% | ||
| Atonic-Astatic | 4/4% | GMFCS 5 | 12/12% |
The body composition study was performed on children over 5 years old using the bioimpedance analysis method [11] with the determination of the following absolute and relative indicators: Fat Mass (FM) and Fat-Free Mass (FFM), Active Cell Mass (ACM), fluid content (total and extracellular), Phase Angle (PA), and Basal Metabolic Rate (BMR).
Statistical processing was performed using the Jamovi 2.6.26 application, employing standard descriptive methods (Me, Q1, Q3), calculation of Pearson's Chi-squared (χ²) for comparing qualitative variables, and the Mann-Whitney U test for quantitative features with a distribution different from normal, considering significance at p < 0.05. Spearman's correlation method was used to assess the strength and direction of the relationship between variables.
Results
The conducted analysis revealed significant differences in body composition among children with cerebral palsy depending on the presence of nutritional insufficiency according to somatometry data. In patients with signs of malnutrition, a decrease in Fat Mass (40%) was significantly more frequent (χ²=4.762; df=1; p < 0.05) – this indicator reflects the degree of development of all adipose tissue, including the visceral component. The Fat Mass Index (FMI) was below normal in 54% of children. Furthermore, even among patients with normal physical development indicators (36%), a decrease in FM (14%) and ACM (18%) was observed, which may indicate hidden trophic status impairments. Increased Fat Mass was found in children without nutritional deficiency and was associated with normal and high anthropometric indicators (p=0.022).
In children with body weight deficit according to physical development assessment, a significant decrease in ACM (p=0.0481) and PA (p=0.0067) was noted. Active Cell Mass reflects the sufficiency of the body's protein pool, and the Phase Angle correlates with the content of metabolically active tissues, allowing their use for assessing nutritional status [12]. Patients in the "red zone" of the table based on body weight had critically low PA (p=0.012), ACM (p=0.013), and iACM (p=0.00228) values. Data analysis established that a decrease in ACM (below -1 SDS) increases the likelihood of protein-energy malnutrition by 1.5 times (95% CI: 0.98-2.47).
Of particular clinical concern is the identification of deviations in body composition in 28.6% of patients with normal anthropometric indicators. Despite the absence of obvious signs of nutritional insufficiency based on physical development assessment, these children showed a decrease in FM (17.9%), FFM (24.6%), ACM (21.4%), and BMR (16%).
In children with severe motor impairments (GMFCS III–V), a decrease in Fat Mass (FM), Fat Mass percentage (FM%), Active Cell Mass (ACM), Skeletal Muscle Mass (SMM), and Fat-Free Mass (FFM) was observed significantly more often (Table 2).
Table 2. Differences in Body Composition in Patients Depending on the Severity of Motor Disorders
| Body Composition Indicators | GMFCS I-II (n=48) Me [Q1; Q3] | GMFCS III-V (n=52) Me [Q1; Q3] | p-value |
|---|---|---|---|
| Fat Mass (FM) | 0.195 [-0.414; 0.948] | -0.255 [-1.159; 0.308] | <0.05* |
| Fat Mass Percentage (FM%) | 0.354 [0.204; 1.198] | 0.023 [-0.362; 0.546] | <0.01** |
| Active Cell Mass (ACM) | -0.817 [-1.744; 0.488] | -1.001 [-2.836; -0.086] | <0.05* |
| Skeletal Muscle Mass (SMM) | 0.574 [-0.250; 1.175] | 0.121 [-0.209; 1.696] | NS |
| Fat-Free Mass (FFM) | -0.568 [-1.446; 0.489] | -0.366 [-1.413; 0.517] | <0.05* |
| Total Body Water (TBW) | -0.721 [-1.613; 0.480] | -0.444 [-1.687; 0.407] | NS |
| *Notes: Data presented as Median [Q1; Q3]. *p < 0.05, **p < 0.01, NS - not significant. Mann-Whitney U test.* |
Dysphagia, leading to impaired nutrient intake, which negatively affects physical development and body composition, can be considered one of the causes of nutritional insufficiency development. According to the study results, children with signs of dysphagia (36% according to the EDACS scale) had significantly lower body composition indicators, including Fat Mass (FM), Fat Mass percentage (FM%), Active Cell Mass (ACM), Fat-Free Mass (FFM), and Phase Angle (PA). Furthermore, the severity of dysphagia demonstrated a direct correlation with the degree of motor limitations on the GMFCS scale (rs=0.82; p < 0.05).
The greatest deviations in body composition indicators (PA, ACM, ACM%) were noted in double hemiplegia (p < 0.05) when compared with spastic diplegia. In the atonic-astatic form of CP, the median values of Phase Angle, Fat Mass, and Active Cell Mass significantly exceeded the corresponding indicators in spastic diplegia.
According to the correlation analysis, direct relationships were determined between PA and FFM (rs=0.226, p < 0.05), ACM (rs=0.331, p < 0.05), SMM (rs=0.218, p < 0.05), and BMR (rs=0.331, p < 0.05). Correlations were found between ACM and body weight (rs=0.950, p < 0.05), height (rs=0.923, p < 0.05), waist circumference (rs=0.822, p < 0.05), and hip circumference (rs=0.914, p < 0.05).
Upon repeated assessment of body composition after 12 [8; 15] months of observation, a significant decrease in Active Cell Mass (ACM), Fat-Free Mass (FFM), and Skeletal Muscle Mass (SMM) indicators was revealed compared to the initial values (see Fig.). These changes correlate with the negative dynamics of physical development [13], manifested by an increase in the proportion of children with signs of malnutrition during the observation period.
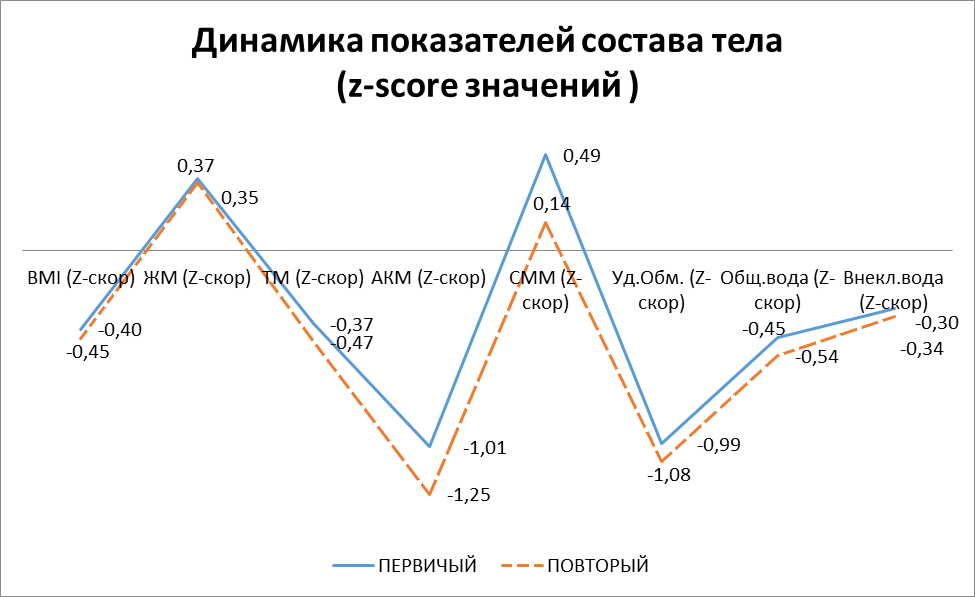
Fig. 1. Dynamics of Body Composition Indicators in Children with Cerebral Palsy
Conclusions
Characteristic changes in body composition indicating nutritional insufficiency were identified in patients with cerebral palsy: a decrease in Active Cell Mass, Fat Mass, and Phase Angle. It should be noted that deviations in body composition are recorded even in children with normal anthropometric indicators. The conducted analysis demonstrated an interrelationship between the severity of motor impairments, the presence of dysphagia, the form of CP, and body composition parameters. A progressive decrease in these indicators over time was noted. The obtained results justify the necessity for regular monitoring of body composition in children with CP as part of comprehensive rehabilitation. This approach ensures the early detection of nutritional disorders and an objective assessment of the effectiveness of the nutritional support provided.
References
1. Gazdieva BM, Puzin SN, Vladimirova ON, Milovanova OA. Level of Primary Disability of Children with Consequences of Infantile Cerebral Palsy. Volgograd Journal of Medical Research. 2024;21(4):12-18. (In Russ.) doi: 10.19163/2658-4514-2024-21-4-12-18.
2. Nezhelskaya A.A., Kurenkov A.L., Kuzenkova L.M., Bursagova B.I. Quality of life in patients with cerebral palsy : literature review. L.O. Badalyan Neurological Journal. 2022;3(3):106-113. (In Russ.) doi: 10.46563/2686-8997-2022-3-3-106-113.
3. Gritsinskaya VL, Novikova VP. Nutritive status of patients with infantile cerebral palsy (review and systematic analysis of publications). Medicine: theory and practice. 2023;8(3):72-81 (In Russ.) DOI: 10.56871/MTP.2023.68.48.007.
4. Zmanovskaya V.A., Levitina E.V., Bunkova S.A., et al. Development of the system for registration and monitoring system for children with cerebral palsy in the Tyumen region (CPUP-Tyumen region). L.O. Badalyan Neurological Journal. 2020;1(2):113-120. (In Russ.) doi: 10.46563/2686-8997-2020-1-2-113-120.
5. Rakhmaeva R.F., Kamalova A.A., Ayupova V.A. Evaluation of anthropometric parameters and body composition in children with cerebral palsy. Rossiyskiy Vestnik Perinatologii i Pediatrii (Russian Bulletin of Perinatology and Pediatrics). 2019;64(5):204-208. (In Russ.) doi: 10.21508/1027-4065-2019-64-5-204-208.
6. Leontiev I.A., Sitnikova E.P., Kovina M.V. Possibilities of using modern standards to assess the physical development of children with cerebral palsy. Children infections. 2024;23(3):30-34. (In Russ.) doi: 10.22627/2072-8107-2024-23-3-30-34.
7. Zavyalova AN. Structure of dysphagia in a pediatric patient and its influence on nutritional status. Prophylactic and Clinical Medicine. 2023;1(86):54-63 (In Russ.) doi: 10.47843/2074-9120_2023_1_54.
8. Plaksina AN, Dugina EA. Nutritive measures as a prerequisite for increasing the effectiveness of rehabilitation of children with cerebral palsy. Child and adolescent rehabilitation. 2016;1(26):16-20 (In Russ.)
9. Brooks J, Day S, Shavelle R, Strauss D. Low weight, morbidity, and mortality in children with cerebral palsy: new clinical growth charts. Pediatrics. 2011 Aug;128(2):e299-307. doi: 10.1542/peds.2010-2801.
10. Palisano RJ, Rosenbaum P, Bartlett D, Livingston MH. Content validity of the expanded and revised Gross Motor Function Classification System. Dev Med Child Neurol. 2008 Oct;50(10):744-50. doi: 10.1111/j.1469-8749.2008.03089.x.
11. Nikolaev DV, Shchelykalina SP. Bioimpedance analysis of human body composition: medical applications, terminology. Clinical nutrition and metabolism. 2021;2(2):80-91 (In Russ.) doi: 10.17816/clinutr72132.
12. Shakurova MT, Vashura AY, Kovtun TA, Sorvacheva TN. Somatic protein pool, muscle mass and sarcopenia as criteria of nutritional status in pediatrics. Treating Physician. 2023; 9 (26): 22-30 (In Russ.) doi: 10.51793/OS.2023.26.9.003.
13. Leontiev IA. Nutritive status of children with infantile cerebral palsy Yaroslavl region, Autoref. diss. ... cand. med. sciences / Leontiev Ivan Andreevich // Smolensk. 2025:23 (In Russ.)
About the Authors
I. A. LeontievРоссия
Ivan A. Leontiev, Assistant Professor
Department of Pediatrics No. 2
Yaroslavl
Competing Interests:
Authors declare no conflict of interest requiring disclosure in this article
E. P. Sitnikova
Россия
Elena P. Sitnikova, Dr. Sci. (Med.), Professor, Head of the Department
Department of Pediatrics No. 2
Yaroslavl
Competing Interests:
Authors declare no conflict of interest requiring disclosure in this article
T. L. Uspenskaya
Россия
Tatiana L. Uspenskaya, Cand. Sci. (Med.), Associate Professor
Department of Pediatrics No. 2
Yaroslavl
Competing Interests:
Authors declare no conflict of interest requiring disclosure in this article
N. V. Olendar
Россия
Natalia V. Olendar, Cand. Sci. (Med.), Associate Professor
Department of Pediatrics № 2
Yaroslavl
Competing Interests:
Authors declare no conflict of interest requiring disclosure in this article
M. V. Kovina
Россия
Marina V. Kovina, Head of the Department, neurologist of the highest qualification category
Department of Speech Pathology and Neuro-rehabilitation
Yaroslavl
Competing Interests:
Authors declare no conflict of interest requiring disclosure in this article
Review
For citations:
Leontiev I.A., Sitnikova E.P., Uspenskaya T.L., Olendar N.V., Kovina M.V. Features of component body composition in children with infantile cerebral palsy. Patient-Oriented Medicine and Pharmacy. 2025;3(3):63-68. (In Russ.) https://doi.org/10.37489/2949-1924-0104. EDN: ZIWMJL
JATS XML


































.png)
